A human apolipoprotein A1 (ApoA1) product, which is the key constituent of high-density lipoprotein (HDL) cholesterol and removes excess lipid from atherosclerotic plaques, did not bring about a significant reduction in the primary endpoint of cardiovascular death, myocardial infarction (MI), or stroke in patients with MI and additional risk factors, in the AEGIS-II trial.
But the trial did show some suggestion of benefit of the ApoA1 product, known as CSL112, with numerically lower rates of cardiovascular death and MI.
In addition, an exploratory analysis showed significant benefits in patients who had higher levels of LDL at baseline, but no benefit in patients with lower LDL levels.
Lead investigator C. Michael Gibson, MD, believes the results of the exploratory analysis are biologically plausible.
“If a patient doesn’t have a lot of excess lipid in their plaques then a therapy to remove lipids from the plaques is not going to help,” he commented.
Gibson, who is professor of medicine at Harvard Medical School, Boston, Massachusetts, said the study results were consistent with the proposed biological action of ApoA1 and HDL plaque stabilization.
And he rejected the idea that the study meant the end of the HDL hypothesis.
“All the steering committee members of the AEGIS-II trial believe these results support the concept of raising ApoA1 or HDL, meaning that the HDL hypothesis is alive and kicking, but it appears that patients need to be hyperlipidemic to benefit,” he said.
Gibson presented the trial results April 6 here at the American College of Cardiology (ACC) Scientific Sessions 2024 in Atlanta. The main results were also simultaneously published online in the New England Journal of Medicine (NEJM).
Study discussant at an ACC press conference, Pamela Morris, MD, who is director of preventive cardiology at the Medical University of South Carolina, Charleston, said the main results of the AEGIS-II study were disappointing.
“The preventive cardiology community will have let out a collective sigh of disappointment with the release of these results,” she said. But she added that the results of the exploratory results are exciting.
“What I take from these results is that we need to be more aggressive in lowering LDL,” she commented.
Morris pointed out that the mean LDL level in study patients was 84 mg/dL, which is higher than current US guidelines for this group of patients.
Gibson noted that some people do not respond to statin therapy and many patients are still hyperlipidemic despite cholesterol-lowering therapy. He suggested that this ApoA1 product may be useful in that group of patients.
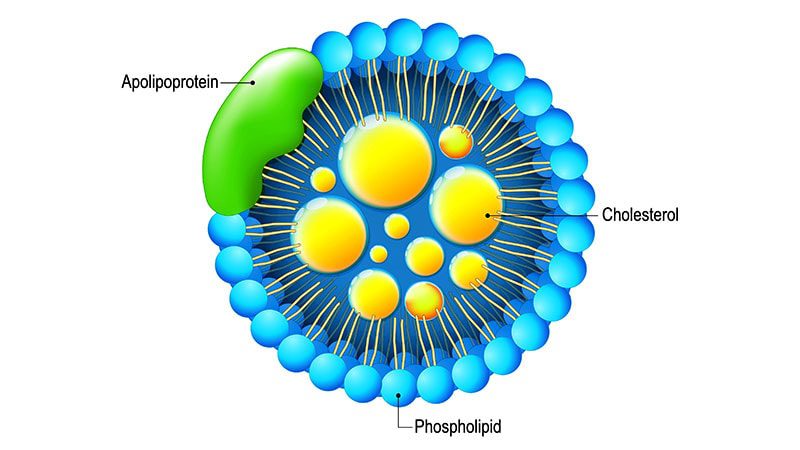
ApoA1 Mediates Cholesterol Efflux
During his presentation, Gibson explained that the disruption of lipid-rich atherosclerotic plaque is often the primary event in acute MI. Reverse cholesterol transport is the mechanism by which excess cholesterol, such as atherosclerotic plaque, is removed from peripheral tissues and transported to the liver for excretion in the bile.
The initial step in reverse cholesterol transport involves cholesterol efflux, which is mediated predominantly by ApoA1. Patients with acute coronary syndrome have an impaired cholesterol efflux capacity, which is associated with a higher incidence of major adverse cardiovascular events.
CSL112 is human plasma–derived ApoA1 given by IV infusion and has previously been shown to boost cholesterol efflux capacity to four times that of baseline.
For the AEGIS-II trial, 18,219 patients with acute MI, multivessel coronary artery disease, and additional cardiovascular risk factors were randomized to receive four weekly infusions of 6 g of CSL112 or matching placebo, with the first infusion administered within 5 days of the MI.
The main result showed no significant difference in the primary endpoint, a composite of MI, stroke, or cardiovascular death at 90 days. The endpoint occurred in 4.8% of the CSL112 group versus 5.2% of the placebo group (hazard ratio [HR], 0.93; 95% CI, 0.81 – 1.05; P = .24).
At 180 days, the endpoint had occurred in 6.9% of the CSL112 group versus 7.6% of those taking placebo (HR, 0.91; 95% CI, 0.81 – 1.01).
At 1 year, the event rate was 9.8% versus 10.5% (HR, 0.93; 95% CI, 0.85 – 1.02).
Further analysis showed that the CSL112 group had a lower number of MI and cardiovascular death events but a higher number of strokes than the placebo group.
When just looking at MI, there was a significant reduction in the CSL112 group at 180 days compared with placebo (5.0% vs 5.7%; HR, 0.87; 95% CI, 0.77 – 0.99; P = .038).
The therapy seemed to be particularly associated with a reduction in early type 4b MI (associated with stent thrombosis) and later type 1 MI.
“Although there was no significant reduction in the incidence of the primary composite endpoint, a positive trend was seen with respect to the individual component of MI that could be consistent with the proposed biologic effect,” the researchers report.
“There was a gradual separation of the curves, with a maximal difference in MI between the two treatment groups at 6 months, which could be consistent with remodeling and subsequent stabilization of atherosclerotic plaque,” they add.
The CSL112 product appeared to be safe, with similar adverse events in the two groups, although there was a higher number of hypersensitivity events reported in the CSL112 group than the placebo group (14 vs 4 events).
In an editorial accompanying the NEJM publication, Christie M. Ballantyne, MD, and Vijay Nambi, MD, Baylor College of Medicine, Houston, Texas, point out that although the AEGIS-II trial showed no clinically meaningful early benefit, the trend towards possible benefit suggests that increasing cholesterol efflux capacity and reverse cholesterol transport may still have potential as a longer-term strategy if medications that can be used over the long term are developed and tested in populations with a decreased cholesterol efflux capacity.
Significant Benefit With High LDL
While presenting the exploratory analysis, Gibson pointed out that there was a positive interaction between the effect of CSL112 and baseline LDL levels.
In patients with baseline LDL levels below 100 mg/dL, there was no effect of CSL112 on the primary composite endpoint at any timepoint.
However, in patients with baseline LDL levels above 100 mg/dL, CSL112 was associated with significant reductions in the primary composite endpoint at all timepoints (Table 1).
Table 1. Incidence of Primary Composite Endpoint in Patients With Baseline LDL > 100 mg/dL
| Timepoint | CSL112, % | Placebo, % | HR (95% CI) | P value |
| 90 days | 3.4 | 4.9 | 0.69 (0.53 – 0.90) | .007 |
| 180 days | 5.3 | 7.3 | 0.71 (0.57 – 0.88) | .002 |
| 365 days | 7.8 | 9.9 | 0.78 (0.65 – 0.93) | .006 |
Gibson said the results of the exploratory analysis make biological sense but need prospective verification.
Commenting for theheart.org | Medscape Cardiology, lipid expert Steve Nissen, MD, Cleveland Clinic, Ohio, described the study as “pretty clearly negative,” adding that it was “disappointing for everyone who wanted HDL to work.”
He said the exploratory analysis suggesting benefit in patients with higher LDL levels was a reasonable hypothesis, but there is always a risk of false-positive results with such post-hoc analyses.
Nissen also pointed out that having a raised LDL level did not necessarily correlate with lipid-laden plaques, so many assumptions were being made.
The AEGIS-II trial was supported by CSL Behring.